Financial, Statistical & Business Related Reports in Dental4Web

A range of reports covering financial, statistical & business, including totals, commissions, production, staff attendance & ADA DelDC survey upload.
Exporting, emailing and printing options available for all reports
Links to 50+ other reports can be found at the bottom of this article thread.
Where to find the Reports page
Click the navigation menu > Management > Reports page
Accounting: Invoices and Receipts Over a Period Report
This report provides detailed information about all the invoices issued: before and after discounts, provider involvement %, expenses, GST, commissions and all the payments received over the selected period of time (including deposits) and refunds for each provider.
Considerations
GST is setup
Provider Commission is setup (if applicable)
Cost to Provider for Expenses is setup if applicable
Prior Period Lock considered
- Double click to open Accounting: Invoices and Receipts over a period
- Report Parameters:
- Date: Select the period to base this report on
- Provider: Select the Provider or <Any Provider>
- Sort By: Select the sort order of the report as Date/Invoice ID/Receipt ID/Name
- Accrual Based: Tick to base report on when transactions occur, not when payments are received
- Show Discount Only: Tick to only show discounts on the report
- Show Totals Only: Tick to remove details from the report
- Group Date Totals: Tick to group totals by date when two or more days are included in the report
- Provider Page Break: Tick to view/print each Providers report on a separate page
- Commissions: Tick to calculate commissions
- Show inactive providers as well: Tick to include Providers made inactive
- Specify Locations
- For Providers/Accounts: Select an individual or all locations
- For Payments/Refunds: Select an individual or all locations
- Click MORE..
- Show data...Main Provider only: Only select this option to base the report on the Main Provider of the patient instead of the Treatment Provider
- Click OK
Report Details
- Dated The date of the invoice and/or receipt.
- Name The name of the patient the invoice and/or receipt refers to.
- Inv/Rec ID The unique number assigned to each invoice and/or receipt generated.
- In/Out Only shown against a patient's name when a deposit has been put against one provider and another provider completes the treatment / uses the deposit.
Invoice Details
- Total The total amount invoiced shown as a $ figure.
- % involved If two providers worked on the one invoice the % involved will be split, otherwise it will show 100%.
- E.g. Provider 1 % involved = 44%, Provider 2 has % involved = 56%.
- $ Discnt The total amount discounted shown as a $ figure.
- $ involved The total amount invoice for after discount and if split by % involved.
- Expense The total of the expense (e.g. Lab) for this invoice/patient on that date.
Receipt Details
- Total The total amount paid on this invoice on that date.
- % involved If two providers worked on the one invoice the % involved will be split, otherwise it will show 100%.
- E.g. Provider 1 % involved = 44%, Provider 2 has % involved = 56%.
- $ involved The total amount paid for that providers % involved.
- Credit/Deposits A positive amount in this field refers to an amount paid, but not allocated to treatment.
- A negative amount in this field refers to a deposit amount allocated to treatment or refunded to patient.
- If allocated to treatment it will show as a receipt against the invoice.
- Discounts (inc. GST) Total amount of discounts given in the period for all providers in the report.
- Promotions (inc. GST) Total amount of promotional discounts given in the period for all providers in the report.
- Expenses (inc. GST) Total amount of expenses paid in the period for all providers in the report.
- Total before discount otal amount received before discounts given.
Invoice Totals
- Invoices (ex. GST) Total invoices for the period excluding any GST.
- GST Total GST involved in invoices for the period.
- Invoices (inc. GST) Total invoices including GST for the period.
Receipts Totals
- Receipts (ex.GST) Total receipts for the period excluding any GST.
- GST Total GST involved in receipts received for the period.
- Receipts (inc.GST) Total receipts including GST for the period.
- Credits/Deposits Total amount of deposits for the period.
- Receipts - Expenses (inc.GST) Nett Total Total receipts minus any expenses based on cost to provider.
- Commission Calculations On Invoices (ex.GST)
- Commission Total commission for this provider based on invoices created excluding GST.
- Calculated as: Invoices x Commission Percentage.
- Expenses Total expenses for this provider based on the Provider Cost for Expenses.
- Comm - Expenses Total commission minus expenses based on invoices created excluding GST.
- Invoices x Commission Percentage – Portion of Expenses provider is responsible for.
- Commission Calculations On Receipts (ex.GST)
- Commission Total commission for this provider based on payments received excluding GST.
- Calculated as: Receipts x Commission Percentage.
- Expenses Total expenses for this provider based on the Provider Cost for Expenses.
- Comm - Expenses Total commission minus expenses based on payments received excluding GST.
- Calculated as: Receipts x Commission Percentage – Portion of Expenses provider is responsible for.
Commission Details on Invoices Raised
The Commission Details on Invoices Raised is used to calculate commission in these circumstances:
Providers are paid based on invoices generated
Providers income is based on a commission calculation from the invoices
It is presumed that commission details have been set for the Provider(s).
- Double click to open the Commission Details on Invoices Raised report
- Report Parameters:
- Date: Select the date range to base the report on
- Location: Select the location or All Locations to base the report on
- Provider: Select the Provider or <All> to include in the report
- Show inactive providers as well: Tick to include inactive provider(s)
- Include Discounts: Tick to include discount details in the report
- Discounts of all periods: When Include Discounts is ticked, tick this box to include discounts of all periods
- Select from the drop list for information to include in the report:
- Item's details: Show items details included in the invoices
- Invoice's details: Show invoice totals only
- Provider summary: Show total for each selected Provider only. When this option is selected, check boxes below will be unavailable
- Provider Page Break: When multiple providers are included in the report, tick to show one provider per page
- Group by providers: When All Locations is selected, tick to group report by provider, instead of by location
- Click OK
Report Details
Depending on the selection from [ABOVE], the report will be viewed one of three ways.
Item's Details View
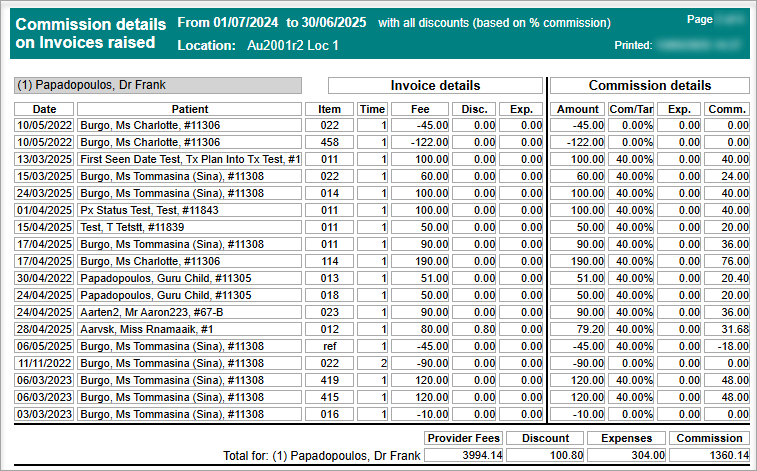
- Date: Date of treatment
- Patient: Patient full name and Card ID
- Item / Time Fee / Disc Exp.: The item performed. How many times
- The fee charged. Any discounts given
- Any expenses relating to the item.
- Amount Total amount for the item
- Comm/Tar The pre-set commission / tariff percentage set up in provider file
- Exp. Any expense costs
- Comm The calculated fee after commission
- Provider Fees Total fee charged
- Discount Total Discounts
- Expenses Total expenses
- Commission Total commission
Invoice Details
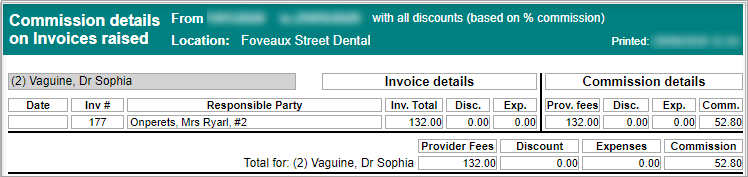
- Date: Date of the invoice
- Responsible Party: Person responsible for the invoice
- Invoice Details: Inv. Total / Disc. / Exp.:
- Total amount for the invoice
- Any discounts given
- Any expense costs within the invoice
- Commission details: Prov.Fees / Disc. / Exp.:
- Provider fees
- Discounts
- Total discounts
- Provider Fees: Total fee charged
- Discount: Total Discounts
- Expenses: Total expenses
- Commission: Total commission
Providers Summary
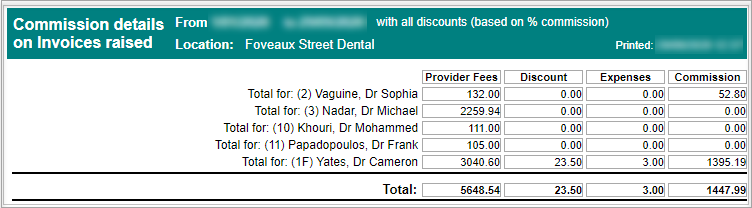
- Total for: A list of all the providers
- Provider Fees: Total fee charged
- Discount: Total Discounts
- Expenses: Total expenses
- Commission: Total commission
Commission Details on Receipts
This report shows commission details of Providers when their income is based on a commission calculated from receipts generated under their names.
- Double click to open Commission details on Receipts report
- Report parameters:
- Location: Select the location or All Locations to base the report on
- Date: Select the date range to base the report on
- Provider: Select the Provider or <All> to include in the report
- Show inactive providers as well: Tick to include inactive provider(s)
- Select from the drop list for information to include in the report:
- Item's details: Show items details included in the receipts
- Receipt's details: Show receipt total only
- Provider summary: Show total for each selected Provider only. When this option is selected, check boxes below will be unavailable
- Provider Page Break: When multiple providers are included in the report, tick to show one provider per page
- Group by providers: When All Locations is selected, tick to group report by provider, instead of by location
- Click OK
Report Details
Show Item's details
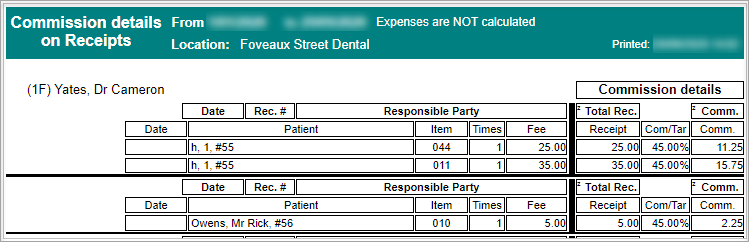
- Date : Date of receipt
- Patient: Patient name and Card ID
- Item / Times / Fee: The item code / How many times / Item fee
- Receipt Com/Tar Comm: Total receipt for the item Commission / Tariff % Commission amount
Show Receipt's details
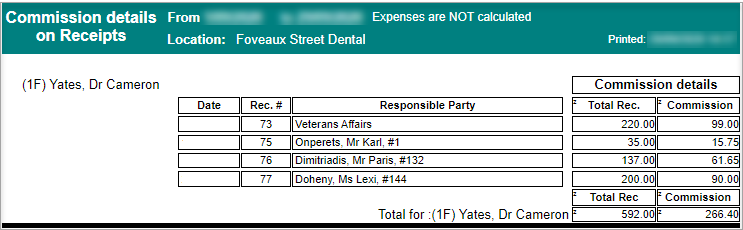
- Date: Date of receipt
- Rec. #: Receipt number
- Responsible party: Person responsible for the payment
- Total Rec.: The total receipt amount
- Commission: The calculated commission amount
- Total For: Name of provider / Total Rec / Commission: The name of the provider / Total receipts / Total commission amount
Show Provider summary
- Total for: Provider (code) and name
- Total Rec: Total Receipts for each provider
- Commissions: Total calculated commissions for each provider
Deposit Allocation Report
This report generates a list of all deposits that have been allocated to an outstanding invoice with details of the percentage and amount involved for each provider.
- Double click to open Deposit Allocation Report
- Report Parameters:
- Date: Select the date range to base this report on
- Location: Select the location to base this report on, if applicable
- Provider: Select the provider(s) to include in the report
- Show inactive providers as well: Tick to include inactive Providers
- Exclude allocations if original payment in this period: Tick to exclude deposits that have been created and allocated in the same reporting period
- Group by Provider: Tick to group allocations by same Provider
- Click OK
Report Details
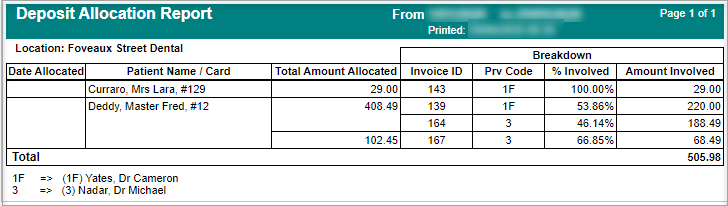
- Date Allocated: The date the deposit was allocated to an invoice
- Patient Name/Card: The patient's name and card number the deposit was from
- Third party name will be shown next to the patient's name if deposit was from a third party
- Total Amount Allocated: The amount of a deposit that has been allocated to an invoice
- Invoiced ID: The invoice ID that the deposit has been allocated to
- Prv Code: The code of the provider whom the deposit has been allocated to
- % Involved: The percentage of the deposit allocated to the invoice
- Amount Involved: The amount of the deposit allocated to the invoice
Discount Categories Report
The Discount Categories Report shows all discounts that have been entered into patients' invoices/receipts over a period of time, separated by the category of discount.
- Double click to open Discount Categories Report
- Report Parameters:
- Date: Select the period to base this report on
- Location: Select the location or <All> to base this report on, if applicable
- Providers: Select the Provider(s) to include in the report
- Show inactive providers: Tick to include inactive Providers
- Show Details: Tick to include details of each account name
- Discount Categories: Select the categories to include
- Show inactive categories: Tick to include inactive Categories
- Click OK
Report Details
Summary View
The report is separated by Providers, then by Discount Category
Show Details View
The report is separated by Providers, then by Discount Category, and includes account name
Efficiency of Referral Sources (Financial Results)
This report generates a list of the financial results for a selected period of time based on referral details.
A referral source must be linked to the patient for the report to generate the correct statistics.
- Double click to open Efficiency of Referral Sources (Financial Results) report
- Report Parameters
- Date: Select the period to base this report on
- Location: Select the location or <All> to base this report on, if applicable
- Providers: Select the Provider(s) to include in the report
- Show inactive providers as well: Tick to include inactive Providers
- Click OK
Report Details
Amounts will only be shown on this report when payment has been received.
No outstanding invoice amounts will be calculated.
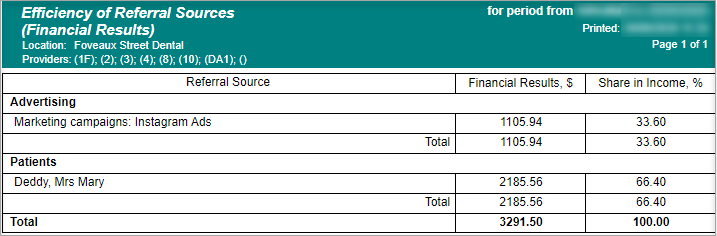
- Financial Results, $: The amount generated from the referral source
- Share in income, %: The % of the overall practice income received
GST Report
This report shows GST information on invoiced item numbers for a selected period of time.
- Double click to open GST report
- Report Parameters:
- Date: Select the period to base this report on
- Location: Select the location or Any Location to base this report on, if applicable
- Show item details: Tick to include details of the items that incurred GST
- Accrual based: Tick to only show invoiced items that incurred GST
- Show ABN Only: Tick to only show information for items that incurred GST
- Show totals only: Tick to show total GST amount only for each provider that belongs to the selected business entity
- Business Entity: Select the Business Entity/ABN to base the report on
- Click OK
Report Details
The report is based on paid item numbers within a selected time period that are inclusive of GST.
- Dated: The date of the item
- Responsible Party: Person/company responsible for the payment
- Account ID: Every invoice has an ID record
- Discount: Any discount given
- GST Due: The amount of GST due
- GST Collected: The amount of GST that was paid
Show item details ticked
Show item details not ticked
Key Performance Indicators Report (Non BIM)
This report shows the total amount of hours setup in Key Performance Indicators for each Provider, along with the total amount of invoices and receipts generated each month for the Provider. The total hours will be divided into productive and administrative hours
The report will work out the average $ amount per hour invoiced and paid to the surgery
- Double click to open Key Performance Indicators Report
- Report Parameters:
- Financial Year: Select Current, Previous or Custom Financial Year to base the report on
- Show totals only: Tick to show total amount only for the selected financial year
- Providers: Mark the tick box to select the Provider(s) to include in this report
- Show Inactive providers as well: Tick to include inactive providers
- Click OK
Report Details
- Monthly: Data in this section are monthly figures
- Cumulative: Data in this section are accumulative figures from the passed months
- Hours: Total amount of hours set in KPI for the Provider. This is not the actual work hour of the Provider.
- Productive (Hrs, %): Total amount of productive hours set in KPI and the percentage it takes in total work hours
- Administr. (Hrs, %): Total amount of administrative hours set in KPI and the percentage it takes in total work hours
- Invoices ($): $ amount of invoices generated in the month for the Provider
- $/Hr: Average $ invoiced per hour
- Receipts ($): $ amount of payment received in the month for the Provider
- $/Hr Average $ payment received per hour
Production Statistics Report
Production Statistics report is used to compare the set production goals per month against issued invoices and money collected.
- Double click to open Production Statistics report
- Report Parameters:
- Financial Year: Select the year to base the report on
- Location: Select the location or <Any Location > if applicable
- Providers: Select the Provider(s) to base the report on
- Show inactive providers as well: Tick to include inactive Providers
- Show Totals Only: Tick to hide the details of the report
- Click OK
Report Details
- For: The Provider the report is based on
- Month: The month the figures relate to
- Production Goal: The previous and current goals from the Providers page
- Actual Issued: The previous and current issued figures
- Collected: The previous and current collected figures
Production from Referral Sources Report
The Production from Referral Sources report calculates the production amounts for different referral sources by the referral date and the production date.
Report Requirements
To capture the referral source, ensure the Referred By feature is used for each patient.
Production contains the total amounts of the patient invoices without discounts.
- Double click to open Production from Referral Source report
- Report Parameters:
- Referral Date: Select the referral period. The referral date is taken from the first seen date
and - Production Date: Select the date. This is based in the invoice date
- Location: Select the location or Any Location to base this report on, if applicable
- Select Providers from the list
- Tick box to include inactive providers
- Click OK
Report Details
- Referral Source: The name of the referral source
- Referral Date: The date of the referral (is set by first seen date of the patient)
- Patient: The Patient details
- Production $: The amount that was invoiced in that period
Receipts on "Hold" from Banking Report
Run the Receipts on Hold from Banking report to view a list of all on hold payments.
- Double click to open the Receipts on "Hold" from Banking report
- Report parameters:
- Location: Select the location to base this report on
- Date: Select the period to base this report on
- Bank Acc: Select the relevant bank account
- Providers: Select the provider(s) to base this report on
- Show Inactive Providers as well: Tick to include inactive providers
- Show Hidden Bank Accounts as well: Tick to include past bank accounts
- Click OK
Report Details
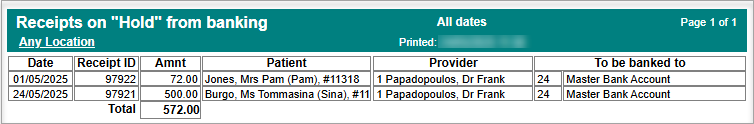
- Date: The date of the receipt
- Receipt ID: The receipt ID automatically generated
- Amt: The amount placed on hold
- Patient: The patient the receipt belongs to
- Provider: The Provider of the patient
- To be banked to: The bank account the receipt should be banked to
Staff Attendance Times
The Staff Attendance Report gathers data entered by staff using the Staff Clock On Clock Off feature.
- Double click to open the Staff Attendance Times report
- Report Parameters:
- Period: Select the period to base this report on
- Location: Select the clinic
- Staff: Select the staff member(s) to report on
- Show inactive staff as well: Tick to include those made inactive
- Print each staff on separate page: Tick to view/print each persons' details on a separate page
- Export to Excel: Tick box if data will be exported
- Click EDIT STAFF ATTENDANCE TIMES if any editing is required to a staff members times (only available to those with access/ editing permission)
- Click OK
Report Details
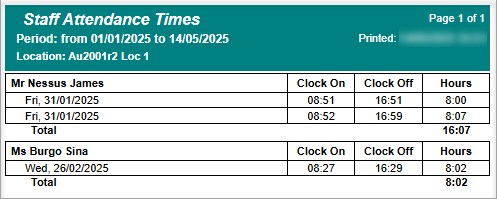
The report will show each time the staff member has clocked on and off with a total number of hours per date.
If a staff member has clocked on and off multiple times in a day the report will show the date multiple times.
The total number of hours worked for the period is shown at the end of the report.
- Staff member: Full name of staff member
- DOW, Date: Day of week, and date
- Clock On: time (24hr) staff member clocked on
- Clock Off: time (24hr) staff member clocked off
- Hours: How many hours worked
- Total: Overall total of hours
Patient List by top paying invoices report
The Patients List by Top Paying Invoices provides a list of the top paying Patients 10 - 500. The report can be group payments by families and/or individual patients.
Considerations
Only receipts that have been allocated to an invoice will be included
Deposits are excluded until they are applied to an invoice
The report period will filter on the date of a receipt, not the date of the invoice
Refunds and Bounced payments will be shown as negative amounts
- Double click to open Patient List by Top Paying Invoices report
- Report Parameters:
- Location: Select the Location, if applicable
- Date: Select the period of payments received to base this report on
- Provider: Select the Provider or <All> to base the report on
- Show inactive Providers as well: Tick to include Providers made inactive
- Family View: Select to group payments by families
- Individual View: Select to show payments per individual patient
- Show top: Select between 10 - 500 patients to show on the report
- Click More if the report should be based on Insurance Funds of the Patients
- Select the Funds to base this report on, or select and tick Exclude Selected Plans to not include them
- Click OK
Report Details
- Patient: The full name and Card Number of the Patient
- Spent: The total amount received for completed treatment for the Patient
- Provider: The Provider(s) of completed treatment which payments were allocated to
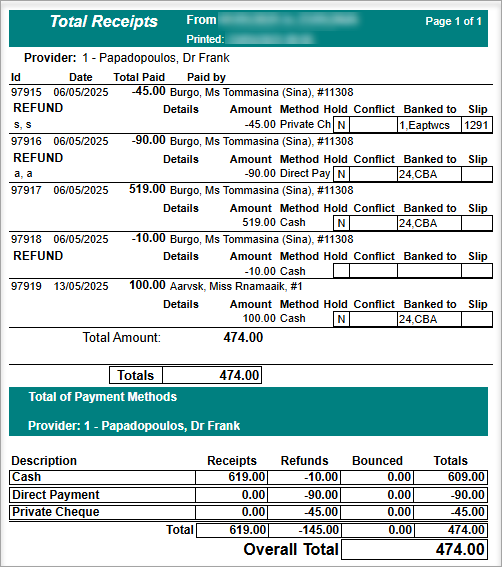
Total Receipts
The Total Receipts Report generates a list of all payments that have been entered within a selected date range.
The report is commonly used for end of day reconciliation and can be run from both the Reports and Bank Slips pages.
- Double click to open the Total Receipts report
- Reports Parameters:
- Location: Select the location or <All> to base this report on, if applicable
- Date: Select the period to base this report on
- Show totals only: Tick to view total amount only - patient details will not be shown in the report
- More: Click to show all payment methods accepted by the practice. You may then select payment method(s) to be included in the report
- Click OK
Report Details
Full Details View
Total Only View
- Description: Payment method used within the report period
- Receipts: Total receipts amount paid via each payment method
- Refunds: Refund given via the payment method
- Bounced: Bounced payment attached to the payment method
- Totals: Total receipts amount after refunds and bounced payments
- Overall Total: Total amount from all payment methods
Total Receipts with Providers
The Total Receipts with Providers Report generates a list of all payments that have been entered within a selected date range, separated by providers. The report can be found in both the Reports and Bank Slips pages.
- Double click to open Total Receipts with providers report
- Reports Parameters:
- Location: Select the location or <All> to base this report on, if applicable
- Date: Select the period to base this report on
- Provider: Select the Provider(s) to include in the report
- MORE: Click to show all payment methods accepted by the practice. User can then select payment method(s) to be included in the report.
- Show inactive providers as well: Tick to include inactive Providers
- Show totals only: Tick to view total amount only - patient details will not be shown in the report
- Show providers from any Location: When a specific location is selected in Location field, tick the box to include providers from all locations
- Click OK
Report Details
Example of Full Details Report
Example of Total Only View
- Description: Payment method used within the report period
Receipts: Total receipts amount paid via each payment method
- Refunds: Refund given via the payment method
- Bounced: Bounced payment attached to the payment method
- Totals: Total receipts amount after refunds and bounced payments
- Overall Total: Total amount from all payment methods
Unallocated Deposits Report
The Unallocated Deposits report allows you to view all deposits for a selected period and provider/s that are yet to be allocated to treatment.
Deposits do not calculate in the accounting report until they are allocated to treatment
- Double click to open the Unallocated Deposits report
- Report Parameters:
- Date: Select the date range
- Location: Select the location or <All> to base this report on, if applicable
- Provider: Select the Provider(s) to include in the report
- Show Inactive Provider as well: This allows you to include providers no longer working at the practice in the report (inactive)
- Tick Payment methods box for individual selection or select all button
- Click OK
Report Details
- Dated: The date of the payment
- Name: The name and card number of the patient
- Payment method: The payment method used by patient
- Inv/Rec ID: The invoice/receipt ID of the payment
- *If a deposit was given to a patient from a Third Party or Guardian then applied against an account, their name will be shown following the patients' name
- Not allocated Deposit - Total: The amount not allocated
Unprinted Invoices Report
This report shows a list of patients where treatment has been performed and entered into the Treatment page but is yet to be invoiced.
- Double click to open the Unprinted Invoices report
- Report parameters:
- Location: Select the location or <All> to base this report on, if applicable
- Provider: Select the Provider(s) to include in the report
- Show inactive providers as well: Tick to include inactive Providers
- Click OK
Report Details
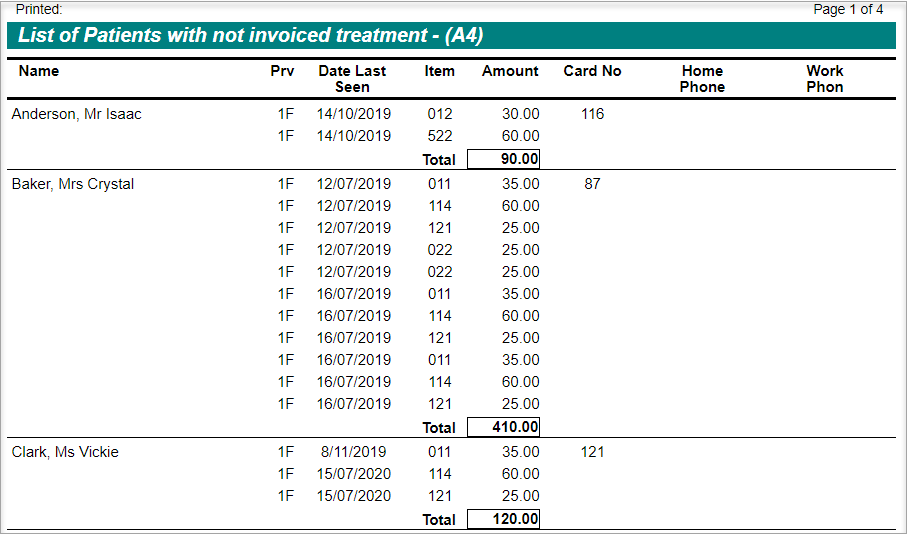
- Name: Patient's name
- Prv: Treatment provider's code
- Date Last Seen: Last seen date of the patient
- Item: The item performed and entered in Treatment tab but not invoiced
- Amount: The amount/fee of the item
- Card No: Patient's card number
- Home Phone: Patient's home phone
- Work Phone: Patient's work phone
Upload ADA DeIDC data file
De-Identified Data Capture (DeIDC) is the system which allows the direct uploading of statistical information from member’s Dental4Web (D4Web) systems to the Australian Dental Association (ADA), eliminating the need for members to respond to the annual fees survey using paper forms manually.
- The paper survey can be inconvenient for members and time consuming for the ADA to process.
- It requires you to fill out a very detailed questionnaire manually, and then the ADA must data-enter it.
The security and privacy arrangements for DeIDC are identical to those for the paper survey. Names and personally identifying information are immediately stripped from the data on receipt.
- We collect names only for the purposes of ‘ticking-off’ members who have responded, and these are discarded and not imported into any database.
- The information we do collect is used only for aggregated statistical processing – ADA Article
Pre-Requisites
- Location Setup
A postcode must be entered for each location of the database. - Click the navigation menu > Location Setup > Location page
- Select the relevant Location if applicable
- Enter the Post Code
- Provider Setup
All providers involved in the ADA survey must be recognised as an ADA Member in D4Web. - Click the navigation menu > Management > Providers page
- Place a tick in the ADA member box
- Repeat for all providers to be included in the survey
- Submit the Survey
- Click the navigation menu > Management > Reports page
- Open Upload ADA DeIDC data file
- Submit New sub-tab
- Location: Select the location to base the survey on if applicable
- Location Type: Select the type of practice
- Customer Ref #: Enter your Centaur Software Customer ID
- Providers: Select the Providers to include in the survey. Those marked as an ADA Member in the Providers tab will automatically select.
- Click SUBMIT
- Click OK to consent or CANCEL to exit
- View Submitted Survey
- Click the navigation menu > Management > Reports page
- Open Upload ADA DeIDC data file
- View Submitted sub-tab
- Date: The date of the survey
- Receipt No: The receipt of the survey submission
- Status
- Successful: The survey was successfully submitted
- Error: See error reasons below
- Error Code 100: Timeout error, suggest to retry submission
- Error Code 200, 300 and 310: Contact Centaur
Related Articles
Financial, Statistical & Business Related Reports in Dental4Windows
A range of reports covering financial data, including totals, commissions, deposits and production. Exporting, emailing and printing options available for all reports Links to 50+ other reports can be found at the bottom of this article thread. Where ...Health Fund & Insurance Reports in Dental4Web
A range of reports covering Health Fund information, H/F claims, Other Insurance and non H/F claiming reports. With exporting, emailing and printing options. Links to 50+ other reports can be found at the bottom of this article thread. Where to find ...Item, Fees & Expense Reports in Dental4Web
A range of reports covering Fee related statistics, Item performance and Expense category reports. With exporting, emailing and printing options. Links to 50+ other reports can be found at the bottom of this article thread. Where to find the Reports ...BIM Reports in Dental4Web
Business Intelligence Module is designed to enhance the analysis & statistic side of reporting. In addition to the numerous standard reports available in D4Web, there are 13 additional reports available here in the BIM. Setup Procedure ...Clinical Reports in Dental4Web
A range of reports covering clinical matters such as Prescription, Treatment Plans, Treatment & Clinical Notes. Exporting, emailing and printing options available for all reports Links to 50+ other reports can be found at the bottom of this article ...
